- male
- 30 Years
- 22/01/2025
I'm really worried about my brother. He had COVID-19 a few months back, and he's still dealing with some tough symptoms like a racing heart rate, tremors, tinnitus, and fatigue. Hes only 30 and was super healthy and fit before all this. His echo was normal a while ago, but the cardiologist did mention arrhythmia back then. Lately, he's been feeling chest pain just from walking or climbing stairs, and his heart rate shoots up to 150-180. It's affecting his daily life a lot post-COVID. We got an NT Pro BNP test done, and it came back at 160. Could this be an early sign of heart failure? Should we look into more tests or anything else?
Answered by 1 Apollo Doctors
"Based on the symptoms your brother is experiencing, along with the elevated NT Pro BNP levels, there may be concerns about the possibility of heart failure. It is important to further investigate and monitor his condition. I recommend consulting with a cardiologist for a thorough evaluation. In the meantime, to help manage his symptoms, he can be prescribed with medication such as Carvedilol 6.25mg twice daily to help reduce heart rate and improve heart function. Additionally, he can take Furosemide 20mg once daily to help reduce fluid buildup in the body. These medications can help alleviate his symptoms and improve his quality of life. It is also important for him to follow a low-sodium diet and avoid strenuous activities. Regular follow-ups with the cardiologist are essential to monitor his condition and adjust treatment as needed."
Dr. Ranjith Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
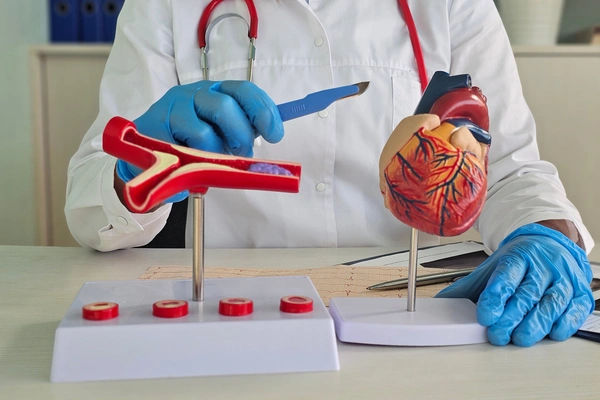
View allI've been wondering about the medication I'm on since I was diagnosed back in January 2013 with a 70% blockage in the LAD due to a rupture plaque. For the past three years, I've been taking Telma H80, Nebicard 5, and Ecosprin av75 daily. I'm curious, how long will I need to continue taking these meds? Are there any additional precautions I should be considering? I walk a lot, about 6-7 km daily, and have no trouble climbing up 3-4 floors of stairs. I'm 40 years old, with a weight of 102 kg, and my blood reports are normal. What do you think?
You have to loose weight and maintain healthy BMI even though the cholesterol is normal for high BMI there is always risk of stroke better to continue to the medication till you are completely normal and healthy in all aspects
Answered by 1 Apollo Doctors
I've been having this burning sensation in the upper back, right at the center, since this morning. It's really bothering me, and I'm not sure if it's something serious or if I'm overthinking it. Could it be a sign of something I should be worried about, or is it just something that happens sometimes? Would really appreciate your thoughts on this.
ecg and cardiac markers are advised to the pt.
Answered by 1 Apollo Doctors
I've had angioplasty with two stents placed back in December 2017. I'm taking Brilinta 90 mg, Carca, Cardace, and Metformin morning and evening, with Ecosprin in the evening. I'm wondering if it's okay for me to have my evening dose of medication after having some alcohol. Is this safe or should I be worried about any interactions?
After consuming liquor, it is generally not recommended to take certain medications due to potential interactions. However, based on the medications you are currently taking, it is safe to take the evening dose of Ecosprin (aspirin) after consuming liquor. It is important to avoid alcohol with Brilinta (Ticagrelor) as it may increase the risk of bleeding. It is also advisable to avoid alcohol with Metformin. As for Carca and Cardace, which are likely beta-blockers and ACE inhibitors respectively, it is generally safe to take them with alcohol in moderation. It is always best to consult with your healthcare provider for personalized advice.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.