- Male
- 31 Years
- 29/01/2025
I'm looking at my lipid profile and I'm a bit worried because my triglycerides are 361. My LDL is at 76, and my HDL is 35. The total cholesterol while fasting came out to 134. I'm not sure what steps I should be taking to bring my triglyceride levels down. Any advice?
Answered by 1 Apollo Doctors
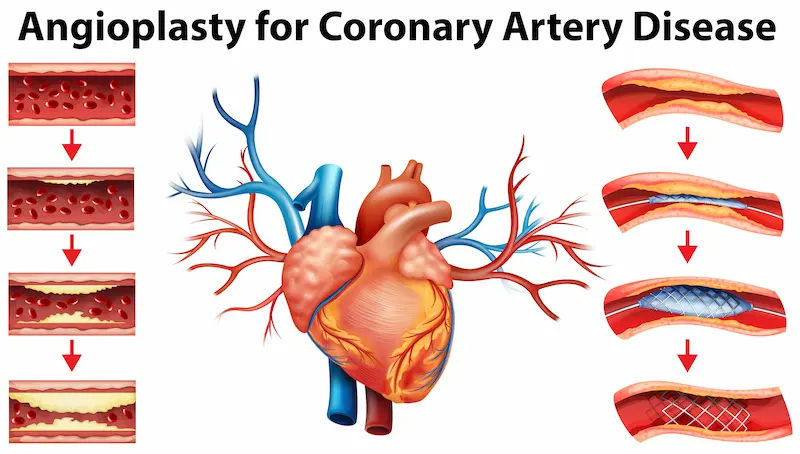
To lower your triglyceride levels, you can start by making some lifestyle changes. You should focus on a healthy diet that is low in saturated fats, trans fats, and cholesterol. Increase your intake of fruits, vegetables, whole grains, and lean proteins. Regular exercise is also important in managing triglyceride levels. In addition to lifestyle changes, your doctor may prescribe medication to help lower your triglycerides. One common medication that is often prescribed for high triglycerides is Fenofibrate. The usual dosage for Fenofibrate is 145 mg once daily. Remember to always follow your doctor's advice and recommendations for managing your lipid profile.
Dr. Ibrahim Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI'm feeling a bit anxious because my heart rate has increased after I took pregabalin. Do you know how long this might last or what I should do next?
After taking pregabalin and experiencing an increased heart rate, it is important to monitor your symptoms closely. The increased heart rate can be a side effect of pregabalin. It is advisable to consult your healthcare provider for further evaluation and management. To address the increased heart rate, you can consider taking a beta-blocker medication such as Metoprolol. The recommended dosage for Metoprolol in this case would be 25-50mg orally once daily. This medication can help lower your heart rate and alleviate the symptoms you are experiencing. The duration of the increased heart rate effect can vary from person to person. It is recommended to continue monitoring your symptoms and consult your healthcare provider if the symptoms persist or worsen.
Answered by 1 Apollo Doctors
I'm really worried because I've been told I have a hole in my heart that can't be cured, and the doctors I've seen said I might not live much longer. Is there anything else I can do or maybe another opinion I should seek? I just want to understand my options better.
Visit your Physician for evaluation and appropriate management
Answered by 1 Apollo Doctors
My dad recently mentioned having a mild chest pain and we found out he has grade 1 diastolic dysfunction. All his other tests came back normal. Should we be worried about this? I've attached his report here. Any advice would be really appreciated.
Reports are normal.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.

_4.webp)

