- female
- 45 Years
- 07/02/2025
I've been having this really awful chest pain for about a month now, and it sometimes feels like my heartbeat is a bit off. After doing a bunch of research, I think it might be esophageal spasms. I went to the ER twice, and they said my EKG and heart monitor were fine. My doctor gave me muscle relaxers, which help with the spasms, but I still cant shake this terrible feeling in my chest. My blood pressure seems okay, it's usually around 120 over 86. I keep feeling my pulse all down my chest and arms, and its been really hard to get any sleep. Could there be something else going on that Im missing?
More Cardiology Health Queries
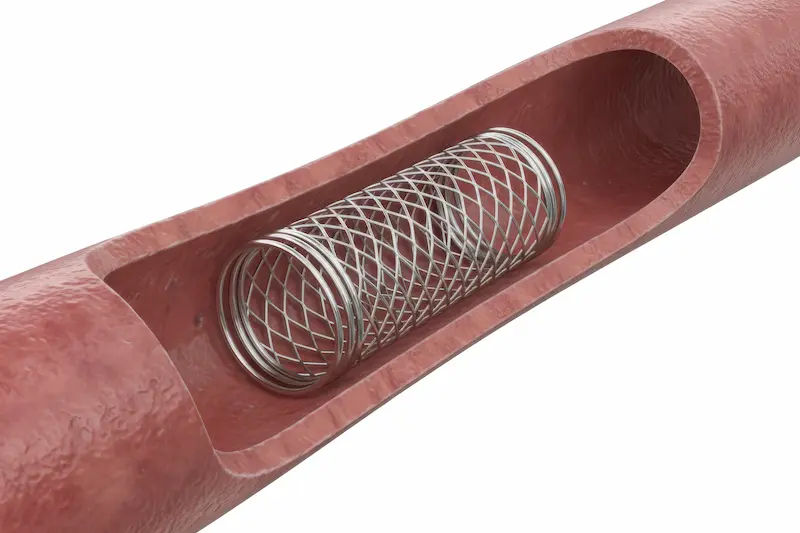
View allMy dad just went through angioplasty a couple of weeks ago and now that he's out of the hospital, I'm really concerned about what kind of diet he should be following. I'm looking for guidance on the best foods he should eat to help with his recovery. Any advice would be really appreciated.
After angioplasty, it is important for your father to follow a heart-healthy diet to promote recovery and reduce the risk of further heart issues. He should focus on consuming a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Some specific foods to include in his diet are: - Oats: High in soluble fiber which can help lower cholesterol levels - Fatty fish like salmon or mackerel: Rich in omega-3 fatty acids which are good for heart health - Nuts and seeds: Almonds, walnuts, chia seeds, flaxseeds are good sources of healthy fats - Berries: Blueberries, strawberries, raspberries are rich in antioxidants - Leafy greens: Spinach, kale, collard greens are packed with vitamins and minerals It is also important for him to limit his intake of saturated fats, trans fats, cholesterol, and sodium. Encourage him to drink plenty of water and avoid sugary beverages. Regular physical activity and stress management are also important components of a heart-healthy lifestyle.
Answered by 1 Apollo Doctors
I've been having chest pains and I got a CT angio which showed myocardial bridging of my proximal LAD at 1.8 cm. My cardiologist said everythings fine and not to worry, but I still get regular chest pains, especially when walking or climbing stairs. What do you think I should do about this?
Based on your symptoms and the presence of myocardial bridging in your proximal LAD, it is important to address the ongoing chest pain you are experiencing. Since your cardiologist has already reviewed your case and deemed it not concerning, you may benefit from medication to help alleviate your symptoms. I recommend starting a calcium channel blocker such as Diltiazem (Cardizem) at a low dose initially, and gradually increasing as needed under the guidance of your doctor. Additionally, you can also consider taking a nitrate medication like Isosorbide Mononitrate (Imdur) to help with chest pain relief during physical activity. It is important to follow up with your cardiologist for further evaluation and management.
Answered by 1 Apollo Doctors
My mom has high blood pressure, and her recent reading was 14090. She's been taking AMTAS daily to manage it, but I'm worried if that reading is still too high. Should we be adjusting her medication or doing something different to get it under control?
Yes,continue same treatment. Salt restricted diet and dash diet is advised to the patient.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.




.webp)