- female
- 50 Years
- 22/01/2025
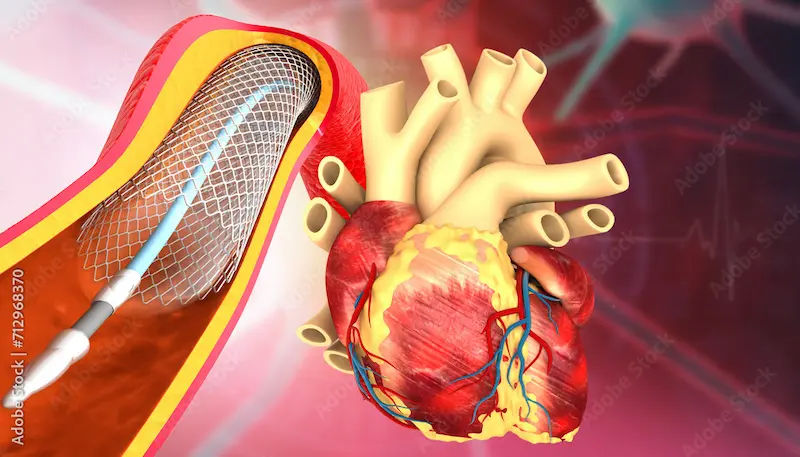
My mom, who's 50, has been taking Thyronorm 50 for her thyroid. Her doctor mentioned noticing some changes in her ECG twice during her follow-ups and suggested she should get a TMT and an Echo done. Her 2D Echo looks normal with an LVEF of 65%, but her TMT came back positive for inducible ischemia at a moderate workload level. She's mentioned having shortness of breath sometimes when she's climbing stairs, but other than that, she's fine and doesn't have any chest pain or a history of high blood pressure or diabetes. What would you suggest as the next steps for her?
More Cardiology Health Queries
View allI'm taking Prolomet 25mg for my high heart rate and blood pressure and I've been on it for about a year. Sometimes when I catch a common cold, it gets hard to breathe and I take Budamet tablets. But when I talked to a pulmonologist, he said that Prolomet isnt good for long-term use because it can cause respiratory issues, and he suggested switching to OLMARK 40 instead. Does this sound right to you, or should I be concerned about making the change?
yes continue olmark 40 medication.
Answered by 1 Apollo Doctors
Is peanut butter good for high blood pressure?
Peanut butter has fiber and proteins which are healthy and few studies showed that it can reduce mean diastolic blood pressure. And as long as they don't contain hydrogenated fat, nut butters including peanut butter won't cause problems for your cholesterol levels too.
Answered by 1 Apollo Doctors
I've been having chest pain for a couple of days now, and it's pretty constant, especially when I'm just sitting or lying down. Plus, sometimes I get this pain in my shoulder and neck, and even occasionally a stomach ache. I'm 20, I don't smoke or drink, and I'm not overweight. Could this be something serious like a heart attack or angina? I'm kinda worried and not sure what to do.
Based on your symptoms and age, it is less likely to be a heart attack or angina. However, chest pain should never be ignored. It is important to rule out any serious conditions. You may be experiencing musculoskeletal pain or acid reflux. I recommend taking over-the-counter antacids like Tums for stomach ache and trying ibuprofen for pain relief. If the symptoms persist or worsen, please consult a healthcare professional for further evaluation and management.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.