- male
- 65 Years
- 20/02/2025
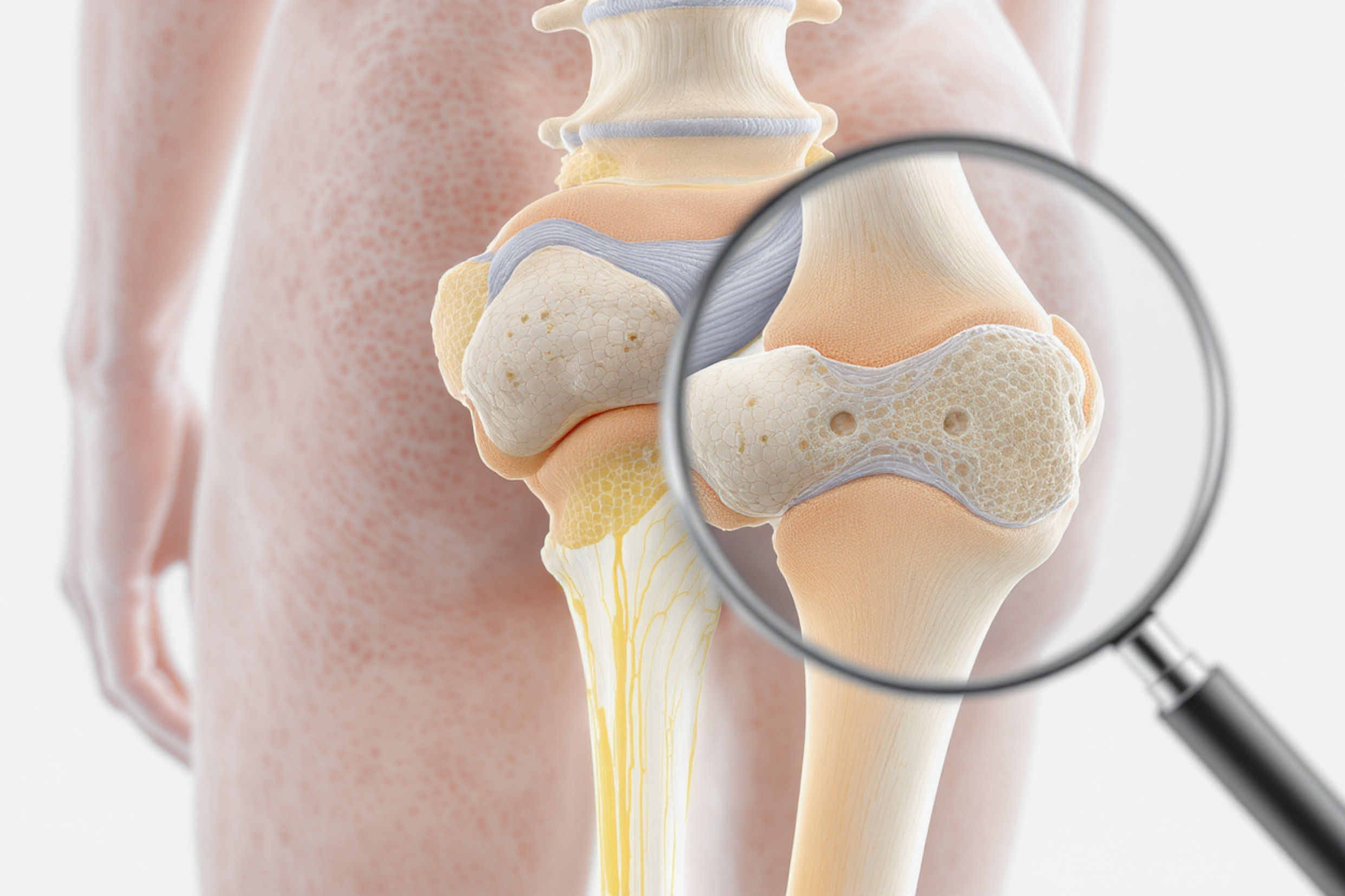
I'm really worried about my dad's blood pressure. It was high at 160110 before, but after he started taking Metocard XL 25 and Triolmesar 20 for about a month, it's dropped to 8772, measured with a digital Omron monitor. Do you think he should keep taking his current medication or adjust the dose? Also, he's diabetic and taking Glyciphage SR 500 and Tenlimac 20. Plus, he's being treated for prostate issues with Maxvoid 8. Could all these medications be affecting his blood pressure too much? What would be the best course of action?
Answered by 1 Apollo Doctors
Given the significant drop in blood pressure from 160110 to 8772, it is important to reassess the medication regimen. In this case, it is advisable to consult with your father's healthcare provider to adjust the dosage or possibly consider discontinuing one of the antihypertensive medications. Lowering the dose of Metocard XL 25 or Triolmesar 20 may be necessary to prevent hypotension, especially considering his current blood pressure readings. Regular monitoring and coordination with his healthcare provider are essential to ensure optimal management of his hypertension while taking into account his diabetes and prostate issues.
Dr. Ranjith Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI'm really worried about my dad he's just 43 and had a heart attack about a month and a half ago. They did an angioplasty and put in a stent, but now the doctor says one of his heart valves isn't working right and needs replacing. His heart is only working at 30% right now. Is it safe for him to go through a bypass surgery at this point, and if he does, how long can we expect him to live after that?
Atleast for a year any surgeries contraindicated.
Answered by 1 Apollo Doctors
I'm 30 and just started working out, but I've noticed during cardio my heart rate goes above 180. Is this normal?
During intense exercise, it is not uncommon for heart rates to exceed 180 beats per minute, especially in younger individuals. However, it is important to monitor your heart rate and listen to your body. If you experience dizziness, chest pain, or difficulty breathing, you should stop exercising and seek medical attention. To help regulate your heart rate during exercise, you can consider taking a beta-blocker such as Metoprolol at a dose of 25-50mg before exercising, after consulting with your doctor.
Answered by 1 Apollo Doctors
I've been experiencing this strange feeling in my heart lately. Its like a drop or a rush of adrenaline, and it's been happening more often. When it does, it really scares me. It's almost like my heart skips a beat or slows down. What could be going on?
Advised an ecg and cardiac markers..
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.