- male
- 60 Years
- 22/01/2025
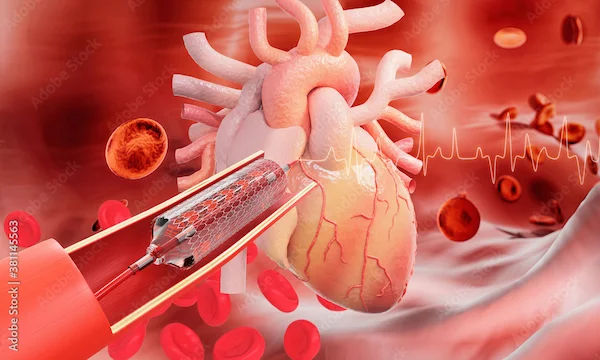
My dad recently had an ECG which turned out normal, but his TMT results showed positive for exercise-induced ischemia. I'm quite worried because his hemoglobin level is really low at 8.8. Do you think he needs an angiogram? I'm not sure what the best next steps are, and would appreciate your guidance.
Answered by 1 Apollo Doctors
Correct anemia first then can think to do stress echocardiography....to confirm..but If there are any risk facters like diabetes and hypertension or smoking or obesity or family history & inactive lifestyle...& symptoms of chest pain or breathing difficulty, angiography should be done Anyways need insight on all these & need to see the TMT strips to suggest the next best step.
Dr. Chandra Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI'm feeling really worried because I've been experiencing chest pain whenever I walk or exert myself. I had a TMT test done, and it was negative. They tried doing a PFT test, but it couldn't be performed. My X-ray came back normal, and the 2D echo showed 60. What could be causing these chest pains despite all these tests being normal? I'm really concerned about what might be happening.
Do Troponin test, need detail history , can guide
Answered by 1 Apollo Doctors
I'm a 29-year-old male with a BMI of 32, and I've been dealing with this weird chest pain for the last 6 to 8 months. It kind of moves around between the right and left side of my chest, and every morning there's this dull pain on the left side that just goes away after a while. It's starting to bug me. Could this be something serious, or is it just normal?
You may be experiencing musculoskeletal chest pain, especially given the fluctuating nature of the pain and the fact that it is more noticeable in the morning and improves throughout the day. However, it's important to rule out any other potential causes of chest pain. Given your age, gender, and BMI, it's important to consider lifestyle factors that may be contributing to your symptoms. I recommend trying over-the-counter pain relievers such as acetaminophen or ibuprofen for relief. Additionally, incorporating regular exercise, maintaining a healthy weight, and improving your posture may help alleviate the chest pain. If the pain persists or worsens, it's important to consult with a healthcare professional for further evaluation and management.
Answered by 1 Apollo Doctors
I'm 22 years old and my blood pressure is 160100. I know I'm obese, could that be causing the high BP? I'm trying to lose weight now.
your obesity is likely contributing to your high blood pressure (HBP), as excess weight can increase blood vessel resistance, cardiac output, and sodium retention; losing weight through a combination of diet, exercise, and lifestyle changes can help lower your BP, aim for a 5-10% weight loss to start
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.