- male
- 30 Years
- 07/02/2025
I've just got my health check-up results and a few things look off, particularly my cholesterol levels. My total cholesterol is 189 mgdl and triglycerides are 249 mgdl, with non-HDL cholesterol at 153 mgdl and VLDL cholesterol at 49.8 mgdl. I'm really concerned about how critical these numbers are and what I should be doing next. Is there a particular specialist I should see, or any specific steps you would recommend for someone my age? I'm 30 and just trying to figure out the best way forward.
Answered by 1 Apollo Doctors
"Based on your lab results, your Total Cholesterol level is 189 mgdl and Triglycerides level is 249 mgdl, which are both elevated. To address this, I recommend starting with lifestyle modifications such as a healthy diet low in saturated fats and sugars, regular exercise, and weight management. In addition to lifestyle changes, you can also consider medication to help lower your cholesterol levels. I suggest consulting with a healthcare provider, such as a cardiologist or a general physician, who can prescribe you a medication like Atorvastatin (brand name Lipitor) at a suitable dosage to help manage your cholesterol levels. Regular follow-up appointments with your healthcare provider will be important to monitor your progress and make any necessary adjustments to your treatment plan. It's also essential to continue monitoring your lipid profile regularly to track your improvement. Remember, these are just general recommendations based on the information provided. It's important to consult with a healthcare professional for personalized advice and treatment."
Dr. Dr Khaleel Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allHey, I've been dealing with this pricking sensation on just the left side of my chest for the past year. It's more like a dull, mild sensation rather than outright pain, and it disappears within seconds. I've already done an ECG, echo, TMT, chest X-ray, and blood tests, and everything came back normal. Do you think I need any more tests to check my heart? Should I be worried about any heart issues even if my tests didn't show anything concerning? Also, what could be causing this pricking feeling in my left chest? Would appreciate your advice.
1) Since your ECG, echo, tmt, chest x-ray, and blood tests have all come back normal, further heart investigations may not be necessary at this point. However, if your symptoms persist or worsen, a coronary angiography may be considered by your doctor. 2) If all your tests have come back normal, it is reassuring and indicates that there may not be a serious issue with your heart. However, it is important to continue monitoring your symptoms and follow up with your healthcare provider regularly. 3) The pricking pain in your left chest could be due to various reasons such as musculoskeletal issues, nerve irritation, anxiety, or gastrointestinal problems. It is important to discuss your symptoms in detail with your doctor to determine the exact cause and appropriate treatment.
Answered by 1 Apollo Doctors
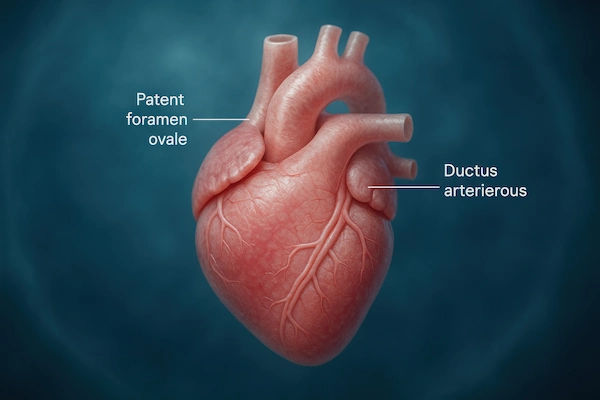
My mom was just diagnosed with a heart valve defect and I'm really worried - does she definitely need open heart surgery or can medicines fix it
cardiologist opinion is advised.
Answered by 1 Apollo Doctors
I've been on Metocard XL 50 for a few months now to manage my hypertension, but lately, my heart rate has been dropping to around 50-52. Could this be because of the Metocard XL 50?
See a specialist for accurate diagnosis and targeted treatment.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.

.webp)