- Male
- 35 Years
- 22/01/2025
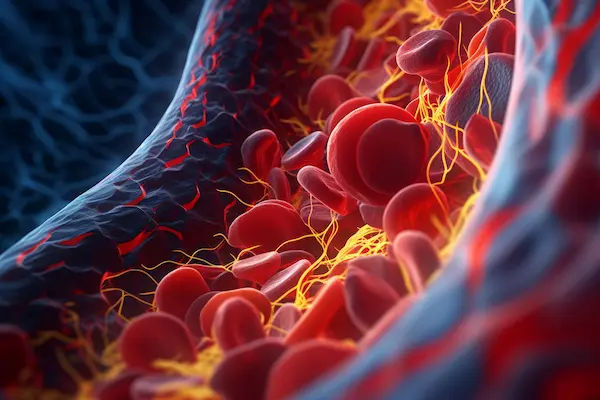
I've been feeling some pain in the middle of my chest, right at the top, for the last couple of months, and it seems to be getting worse every day. I've also been dealing with catarrh for a few years now. Could these be related, and should I be worried about this chest pain getting worse?
More Cardiology Health Queries
View allHow long are ECG, 2D ECHO, and Stress ECHO results valid? I've done these tests and everything came back normal, but I'm curious about how long these results are considered accurate. Should I repeat them often or are they good for a while?
Echo is valid for 6-12 months.
read more![Doctor 1]()
![Doctor 2]()
Answered by 1 Apollo Doctors
I've been dealing with a dry cough after starting Cardace 2.5 mg following a heart attack last month. I'm also on Brillinta, Concor, and Ecospirin. Is this cough something I should be worried about, or should I think about stopping Cardace?
continue the same medications, all medications to be continued.. cough is the side effect nothing to worry..
read more![Doctor 1]()
![Doctor 2]()
Answered by 1 Apollo Doctors
What does it mean when bronchovascular markings are seen in the right paracardiac region on a chest X-ray? Is this something I should be worried about?
suggestive of cardiac infection advised an ecg and cardiac markers for the diagnosis of any pathological anomaluy..
read more![Doctor 1]()
![Doctor 2]()
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.


.webp)


.webp)