- male
- 50 Years
- 22/01/2025
I'm worried because my blood pressure has been 14090 for the past 20 days, and I've started having mild chest pain. I've done all the heart-related tests like ECG, echo, and TMT, and they all came back normal. Should I be taking blood pressure medicine? My doctor hasn't prescribed anything for it yet, but I'm thinking maybe I should start at least for a few days. I weigh 110 kg, and my doctor only put me on cholesterol medication since my cholesterol is high. What do you think about starting bp medicine?
Answered by 1 Apollo Doctors
Your blood pressure reading of 14090 mmHg falls into the category of Stage 1 Hypertension according to most guidelines Since your heart-related tests (ECG, ECHO, TMT) are normal, and your doctor has not prescribed blood pressure (BP) medication, they may believe that your condition can initially be managed with lifestyle changes and monitoring. However, your weight (110 kg) and high cholesterol are additional risk factors for cardiovascular disease, and managing your blood pressure is crucial.
Dr. Ranjith Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI'm experiencing some chest pain and chest congestion, especially on the left side of my chest. It's been really uncomfortable and I'm not sure what's going on. Can you help me understand what's causing this and what I should do next?
take tablet zerodol for 5 days
Answered by 1 Apollo Doctors
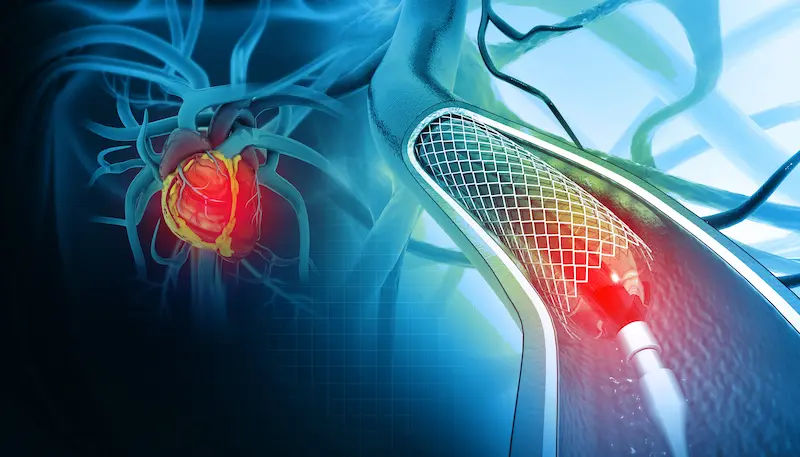
I'm really concerned because my heartbeat is only 20 and I'm having trouble breathing. Can you tell me how much your EECP treatment costs? How long does the treatment usually take? And could you walk me through the whole treatment process? I'm eager to understand more about what to expect.
For your condition, EECP (Enhanced External Counterpulsation) treatment can be beneficial. The treatment fee can vary depending on the healthcare facility and location, so it's best to inquire directly at the clinic. Typically, an EECP treatment course involves 35 one-hour sessions, usually conducted over a span of 7 weeks (5 sessions per week). During the treatment process, you will be comfortably lying on a bed with large blood pressure-like cuffs wrapped around your legs. These cuffs will inflate and deflate in sync with your heartbeat to increase blood flow to your heart and improve its function. This non-invasive treatment can help improve your heart function and alleviate symptoms like shortness of breath. I hope this information helps.
Answered by 1 Apollo Doctors
I'm trying to understand the results of my recent 2D echo and colour Doppler test. It mentioned things like LEFT VENTRICLE ASH, TRILEAFLETS, and an AORTIC VALVE that's thickened. It also noted some stuff about COLOUR DOPPLER and something called AV GRDT 5mmHg AR GRADE 1. They concluded I have HYPERTENSIVE HEART DISEASE and ASYMMETRICAL SEPTAL HYPERTROPHY among other things. They said I have a NORMAL LV SYSTOLIC FUNCTION with an EF of 64%, but I'm not quite sure what that means. Given this, is my condition something thats curable or can be managed? Would surgery or implants help at all? I don't have diabetes and my heart rate stays around 50-60 bpm consistently. I've been on Zabeta X for nine years, then LODOZ 2.5 for a year, and now CONCOR 2.5 for the last 15 days. Also, I've been taking Restyl 0.5 at bedtime for 9 years. What should I consider doing next?
1. Whether it is curablecontrolled? Based on the diagnosis of hypertensive heart disease, asymmetrical septal hypertrophy, sclerotic aortic valve with mild aortic regurgitation, and left ventricular diastolic dysfunction, these conditions can be managed and controlled with appropriate treatment and lifestyle modifications. While these conditions may not be completely curable, their progression can be slowed down and symptoms can be managed effectively with proper medical management. 2. Whether surgery or implants in any way will be of any help? In your case, since you have normal left ventricular systolic function and no regional wall motion abnormalities at rest, surgery or implants may not be necessary at this point. However, in some cases where there is severe aortic stenosis or regurgitation, surgical interventions such as aortic valve replacement may be considered. It is important to follow up with your cardiologist for further evaluation and to determine if any surgical interventions are needed in the future. 3. Your considered opinion, suggestion, solution? Considering your current medication regimen, it is important to continue taking Concor 2.5 as prescribed by your healthcare provider. Additionally, lifestyle modifications such as maintaining a healthy diet, regular exercise, managing stress, and avoiding smoking can help in managing your condition. Regular follow-up visits with your cardiologist are essential to monitor your heart health and adjust your treatment plan as needed. If you have any concerns or experience any new symptoms, please consult your healthcare provider for further evaluation and management.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.


_1.webp)
