- Male
- 62 Years
- 29/01/2025
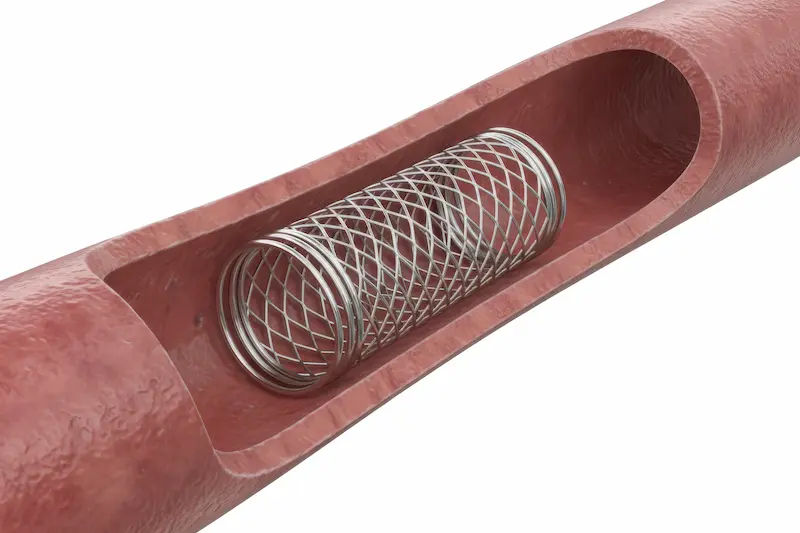
I'm really worried about my 62-year-old diabetic relative. He's had angina for over a year, and his ECG showed some troubling signs like a Q wave with T wave inversion. The echocardiogram was apparently normal, but the treadmill test came back positive, and the coronary angiogram revealed triple vessel coronary artery disease. He's stable now, thankfully, but they recommended PCI for the LCx and RCA. I'm just wondering what all this really means and where would be the best place for him to get this treatment? I'm feeling a bit lost here.
More Cardiology Health Queries
View allMy dad is 58 and has a lot going on with his health. He's been through CABG surgery and deals with CKD and diabetes. His weight is around 59-61 kg. Up until now, his blood pressure's been quite stable, but recently I noticed it's gone up to about 140150 over 8090. I'm getting pretty worried about it. Do you think there's something with his medication? He's on Orofer XT, Cardivas 6.25, Nefrosave forte, Alfoo tab, Ecospirin Gold, and Isolazine. Could any dietary changes help as well? Would love to know what you think.
Given your father's medical history and current medications, to help manage his increased blood pressure, you can consider adding an antihypertensive medication like Amlodipine 5mg once daily. Additionally, it's important to ensure he is following a low-sodium diet, rich in fruits, vegetables, and whole grains. Encouraging regular physical activity and stress-reducing activities can also be beneficial for his overall health.
Answered by 1 Apollo Doctors
Heart function is less than fifty percent, which is pretty concerning. I'm wondering how I can improve it. Is it possible to fix this with medicine alone, or would I need something like a stent or another type of treatment? Any advice would be appreciated!
i means that there is systolic dysfunction or acute angina, papillary muscle dysfunction or any heart blocks..i would suggest an angiogram procedure to the patient to look into any pathological defects..Patient is advised DASH Diet , low sodium intake, consumption of green leafy negetables,fruits and legumes etc..
Answered by 1 Apollo Doctors
I'm really concerned about my cholesterol levels. I had really high LDL cholesterol at 293, but after taking medications like Rosuvastatin, changing my diet, and exercising more, my bad cholesterol has apparently gone down to normal. I'm wondering though, since high bad cholesterol is known for causing blockages in arteries, does it mean I'm in the clear now that my levels are normal? Or should I still be worried about any existing blockages?
After reducing your bad cholesterol levels with Roseday 10, diet, and exercise, it is likely that the risk of blockages in your arteries has decreased. However, it is important to continue with a healthy lifestyle to maintain these improvements. Regular monitoring of your cholesterol levels is also recommended to ensure they stay within a healthy range.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.



.webp)
_1.webp)