- Male
- 34 Years
- 22/01/2025
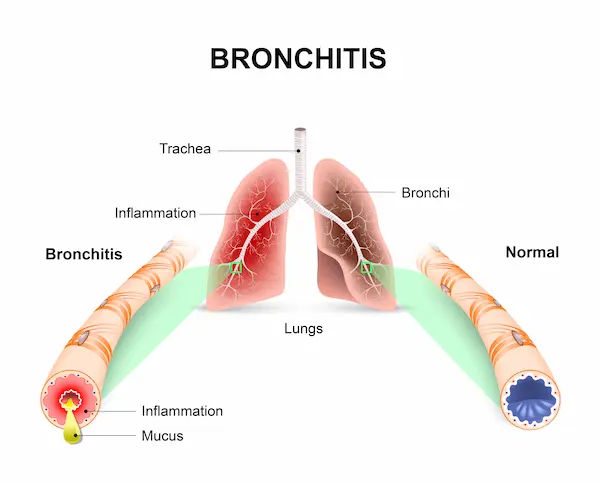
I'm really concerned about my husband. He tested positive for COVID-19 back on May 17, 2021, and it's been over three months since then. On May 24th, a CT scan showed he had 25% lung involvement. He was on oxygen support for a month and got discharged on June 22, 2021, so it's been about two and a half months now. His oxygen level is around 98-99 when he's just sitting, but when he does brisk walking or climbs stairs quickly, his breathing gets faster for a couple of minutes, and then settles back down. During this time, his oxygen saturation levels drop to about 89-93 for a few seconds before going back up to 99 and staying there. Is this something we should be worried about? Also, he sometimes gets a dry cough a few times a day and feels a mild chest pain then. His respiratory rate is around 20-22 bpm. Are these symptoms normal or is there something we should be looking into? I'm really anxious about all this.
More Pulmonology/ Respiratory Medicine Health Queries
View allIve been dealing with shortness of breath for about 5 years and all my tests like PFT, ECG, CT thorax, chest X-rays, 2D echo, and others came back normal. Ive even had them repeated in 2017 and 2019. Ive seen a lot of pulmonologists and cardiologists but nobodys been able to figure it out. It used to only bother me at night but now it happens during the day too. Even sleep meds arent helping now. Some doctors thought it was tension or weakness, but I'm quite active, exercising and doing yoga and pranayama daily. Night times are really tough and sometimes I can't sleep at all, even with meditation or taking stalopam plus. I'm only 21, so its really worrying. What do you think could be going on?
continue doing yoga , if still not resolved consult a pulmonologist
Answered by 1 Apollo Doctors
I'm really concerned about my mom's recent x-ray report. It shows that both of her hila are congested. She had breast cancer about five years ago and went through surgery and chemotherapy, but has been doing well since then. Now with this new x-ray showing congestion and her having some breathing problems, I'm pretty worried. Can you help me understand what this might mean?
Visit your Physician for appropriate management
Answered by 1 Apollo Doctors
I recently had a chest X-ray and it came back saying that there are prominent bilateral hilar shadows. I'm a bit worried and would really like to understand what this means. Could you explain it to me?
Bilateral Hilar Shadows being prominent on your chest X-ray typically indicates enlargement or prominence of the lymph nodes in the hilar region of the lungs, which can be caused by various conditions such as tuberculosis, sarcoidosis, lymphoma, or other inflammatory or infectious diseases, and further testing or evaluation by a specialist is usually required to determine the underlying cause.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.