- male
- 45 Years
- 20/02/2025
I'm experiencing some mild pain in my upper chest on both sides and also in my upper back, and sometimes even in the lower part of my chest. I went to the doctor yesterday, and he did an ECG, which came back normal. My oxygen level is 97, but I'm still feeling like I need to take a deep breath every 10 minutes or so, and Im not sure why. Could you help me figure out what's going on?
Answered by 1 Apollo Doctors
do chest x ray
Dr. Anshul Suggests...
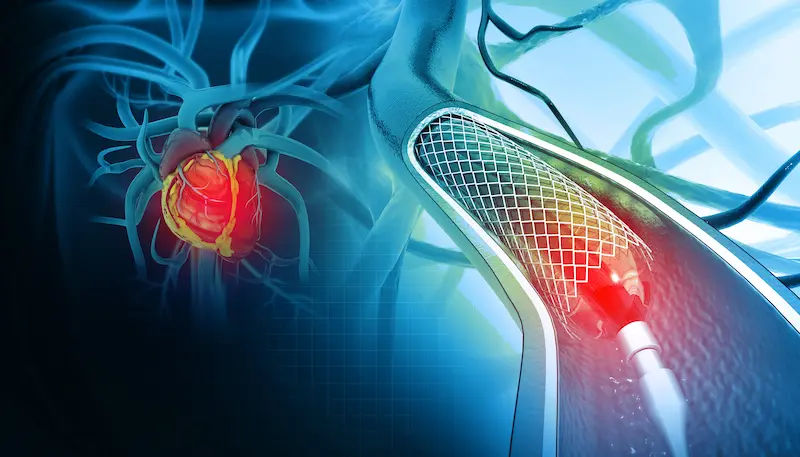
Consult a Cardiologist
Answered 04/07/2025
0
0


Ask Apollo
AI powered Health Chatbot
-
Possible Causes
a. Musculoskeletal issues: Consider muscle strain or tension.
b. Anxiety or stress: Can cause similar symptoms.
c. Gastroesophageal reflux: May lead to chest discomfort. -
Immediate Actions
a. Practice deep breathing exercises to manage breathlessness.
b. Use over-the-counter pain relief if needed, following package instructions. -
When to Seek Further Medical Attention
a. If symptoms worsen or new symptoms develop.
b. Persistent or severe pain despite initial measures. -
Follow-Up
a. Schedule a follow-up with your doctor if symptoms persist.
b. Discuss any lifestyle factors that may contribute to symptoms.
Answered 10/09/2025
0
0
More Cardiology Health Queries
View allI've been having this regular pain on the left side of my chest for about a week now, and after getting some cardiac tests done, they mentioned things like Sinus bradycardia with Sinus arrhythmia and Hyperacute T waves. I'm having some breathlessness too, but my heartbeat is at 58. The TIPI probability of ACI came out as 9. I'm really hoping you could help me understand what all of this means and if it's something I should be really worried about. Would love some guidance on this!
kindly visit a cardiologist
Answered by 1 Apollo Doctors
I've been dealing with moderate hypertension since I got diagnosed with a BP of 168122 on December 18th, and I've been put on Telma 40. But for the past three days, I've been having this awful headache and pain in my cheek, only on the left side of my face. My blood pressure is still at 150115 even though I've been taking the medicine for these three days. Should I be concerned about this, and what should I do next?
Given your recent diagnosis of moderate hypertension and the current blood pressure readings of 150115 despite taking Telma 40 (telmisartan), it is essential to address this promptly. Your persistent headache and left-sided cheek pain might indicate uncontrolled hypertension, which can lead to severe complications if not managed appropriately. Firstly, I recommend you seek immediate medical attention to evaluate your symptoms. Your healthcare provider might need to adjust your blood pressure medication or add additional antihypertensive agents to better control your blood pressure. They may also want to investigate the cause of your headache and cheek pain to rule out other potential issues, such as sinusitis or trigeminal neuralgia. In the meantime, continue taking your medication as prescribed and avoid any activities that could elevate your blood pressure further. Please contact your healthcare provider as soon as possible to discuss these symptoms.
Answered by 1 Apollo Doctors
I'm really worried about my dad. He's been taking ecosprin AV but he's been having some abdomen pain, so the doctor suggested a USG, and they also mentioned theyll do a TMT test. In the meantime, they've switched his medication from ecosprin AV to a mix of Telmisartan and Metaprolol Succinate until they can do the TMT test. Unfortunately, we couldn't get the USG and TMT tests done today. Is it safe for him to stop taking ecosprin AV for now?
it is advisable to follow your doctor's instructions regarding medication changes. In this case, since your father's medication has been changed from Ecosprin AV to Telmisartan and Metoprolol Succinate combination, it is important to continue with the new medication as prescribed. Once the TMT test and USG are conducted, the doctor will be able to provide further guidance based on the results. It is generally not recommended to stop medication abruptly without consulting the doctor. Therefore, please continue with the Telmisartan and Metoprolol Succinate combination as advised by the doctor
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.

 Could muscle strain cause my chest pain?
Could muscle strain cause my chest pain?