- Male
- 28 Years
- 29/01/2025
I'm experiencing some heart-related issues that are making me a bit anxious. Back in December 2019, I had a fast heartbeat and some pain on my left side, so I went to a cardio doctor in Patna. After running an ECG, he prescribed me clonozepam, etizola, and a beta blocker, which really helped at the time. But lately, I've been noticing this fluttering sensation in my heart, and it's making me wonder if it's something I should be worried about or if it's fine to just ignore it. Could you give me some advice on this?
More Cardiology Health Queries
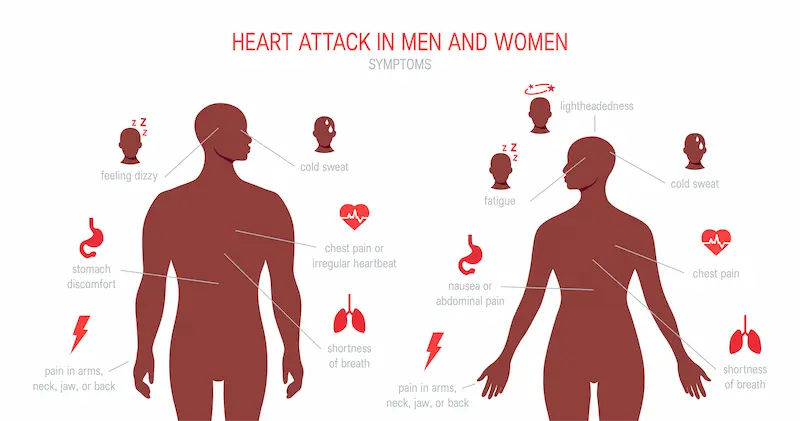
View allI've been having some pain in my left arm and numbness in my chest today, and my ECG results say there's a suspected inferior infarction. I'm really worried about what this means. Is this something that can be reversed or cured? And what kind of treatment would I need for this?
Inferior infarction refers to a heart attack that affects the inferior wall of the heart. It is a serious condition that requires prompt medical attention. Treatment for inferior infarction typically involves medications to reduce the workload on the heart and prevent further complications. Common medications used in the treatment of heart attacks include: - Aspirin 325mg to reduce blood clotting - Clopidogrel 75mg to prevent blood clots - Nitroglycerin to improve blood flow to the heart - Beta-blockers like Metoprolol to reduce the workload on the heart - ACE inhibitors like Lisinopril to improve heart function - Statins like Atorvastatin to lower cholesterol levels It is important to follow your doctor's recommendations for treatment and lifestyle changes to manage and prevent future heart issues.
Answered by 1 Apollo Doctors
I'm trying to understand my recent test results. I have Atrial Fib, and although my last stress test didn't show any blockage, there was something like a shadow at the bottom of my heart. What could this shadow mean?
Diagnosis - is atrial fibrillation u can continue medications antiarrythmics,anticoagulants,cardioversion,catheter ablation, beta blocker and calcium channel blockers.
Answered by 1 Apollo Doctors
I'm feeling this sharp pain in my chest and the backside of my shoulder, especially when I stretch or take a deep breath. I had COVID-19 last year, but I've fully gotten over that. I seem to catch colds pretty often too. Can you help me figure out what's going on?
take tablet . citrizen and tablet. pantoprazole it will relieve your symptoms
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.