- male
- 50 Years
- 31/03/2021
Does your body warn you before a heart attack?
Answered by 1 Apollo Doctors
Yes the warning signs are Pressure, fullness, squeezing pain in the center of the chest, spreading to the neck, shoulder or jaw along with Light-headedness, fainting, sweating, nausea, or shortness of breath with or without chest discomfort, upper abdominal pressure or discomfort.
Dr. Kareemulla Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0


Ask Apollo
AI powered Health Chatbot
-
Common Warning Signs Before a Heart Attack
- Sudden chest discomfort, shortness of breath, and unexplained sweating.
-
Less Typical or Atypical Symptoms
- Fatigue, nausea, or pain in the jaw, neck, or back.
-
Importance of Recognizing Symptoms Early
- Early recognition is crucial for timely medical intervention.
-
When to Seek Immediate Medical Help
- Seek urgent care for severe chest pain, sudden sweating, or shortness of breath.
-
Relevant Medical Specialties and Tests
- Consult a cardiologist; tests like ECG or blood tests can confirm a heart attack.
-
Preventive Measures and Lifestyle Advice
- Adopt a healthy lifestyle and schedule regular check-ups to reduce risk.
Recommended next steps
Consult a Cardiologist or Take a CBC Test (Complete Blood Count) Test
Answered 20/08/2025
0
0
More Cardiology Health Queries
View allI'm really worried about my dad's health. He's been diabetic since 2003 and had a CABG in 2008. He's got moderate LVF dysfunction and was in and out of the hospital in 2015 and early 2016 because of pulmonary edema. He's also dealing with hypothyroidism and recently his serum creatine levels increased, so he's on a renal diet and taking a bunch of meds for diabetes, insulin, heart, and thyroid. Lately, since January 2016, he's losing weight and gets short of breath really easily, like after walking just 10-15 meters. His latest blood tests showed low potassium, so the doc gave him a tonic for that. But now he's feeling weak and says he can't taste his food right sometimes. I'm at a loss herehow can we improve his health condition?
Your father's health condition is complex, but based on the symptoms described, it seems like he may be experiencing symptoms of electrolyte imbalance, which could be contributing to his weakness and altered taste sensation. In addition to the tonic for increasing potassium, I would recommend adding a potassium supplement such as Slow-K (Potassium Chloride) to help normalize his serum potassium levels. The usual dosage is 20 mEq to 40 mEq daily, but this should be adjusted based on his specific needs and blood test results. To address his shortness of breath and symptoms of heart failure, his doctor may consider adding or adjusting medications such as Lasix (Furosemide) to help reduce fluid buildup in the lungs and improve breathing. The dosage will depend on his current medication regimen and kidney function. For his thyroid condition, ensuring that he is taking his thyroid medication regularly and having regular follow-ups with his endocrinologist is important to optimize his thyroid hormone levels. Given his history of diabetes, heart issues, and kidney problems, it's crucial for his healthcare team to closely monitor his kidney function and adjust his medications as needed to prevent further complications. Overall, it's important for your father to continue following his renal diet, taking his medications as prescribed, and attending regular follow-up appointments with his healthcare providers to manage his multiple health conditions effectively.
Answered by 1 Apollo Doctors
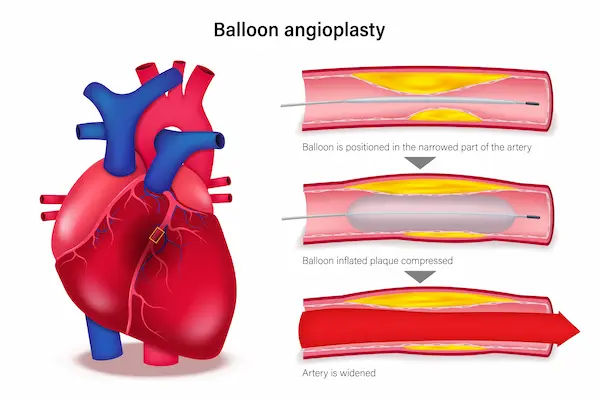
My dad's treadmill test results came back with a positive result, and the doctor mentioned he might need an angiography. The TMT report shows an ST depression of 1.5 to 2 mm. I'm really concerned about what this all means. Is this depression considered mild, or does it indicate a high possibility of blockage?
The ST depression of 1.5 to 2 mm on the TMT report indicates a moderate level of ischemia, suggesting a significant possibility of blockage in the coronary arteries. It is important to follow up with the angiography as recommended by the doctor to further evaluate the extent of blockage and determine the appropriate treatment. In the meantime, medications like Aspirin 75mg and Clopidogrel 75mg can be prescribed to reduce the risk of clot formation.
Answered by 1 Apollo Doctors
I'm really worried about what it means to have a normal ECG but still have a short PR interval. Could having a short PR be dangerous enough to cause life-threatening arrhythmias? I'm not sure if this is something I should be really concerned about or if its common for my situation. Can you help clarify this for me?
yes ,cardiologist opinion is advised.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.