Diabetes Management
Gestational Diabetes: Symptoms, Causes, Diagnosis, Treatment & Prevention
10 min read
By Apollo 24|7, Published on - 04 July 2023
Share this article
0
0 like

Gestational diabetes (GD) is a condition marked by high blood sugar levels during pregnancy. It usually occurs between the 24th and 28th weeks of pregnancy. Getting diagnosed with gestational diabetes doesn't mean the person had diabetes before conceiving. Similar to other forms of diabetes, GD affects the utilization of sugar (glucose) in the cells. Gestational diabetes can affect the health of both the mother and the baby. Though, in most cases, gestational diabetes resolves on its own after giving birth, doctors monitor the woman's blood sugar shortly after delivery and again within six weeks. Read on to learn more about the symptoms, diagnosis, and treatment of gestational diabetes.
Gestational Diabetes Symptoms
Gestational diabetes often does not exhibit any noticeable warning signs. The symptoms are typically mild and can easily go unnoticed until you undergo diabetes testing during the second trimester of your pregnancy. However, some individuals may experience symptoms like:
- Nausea
- Frequent urination
- Excessive thirst
- Tiredness
- Frequent bladder, skin, or vaginal infections
- Blurred vision
Gestational Diabetes Causes
The hormone insulin is responsible for breaking down food into glucose and transporting it to cells for energy production. However, if insulin functions improperly or is insufficient, glucose accumulates in the blood, resulting in diabetes.
During pregnancy, hormonal fluctuations can interfere with insulin's effectiveness, causing gestational diabetes. Additionally, genetic factors and being overweight (having a BMI greater than 25) may also contribute to its development.
Gestational Diabetes Risk Factors
Gestational diabetes can occur in any pregnant individual. Though the exact reason for gestational diabetes is still unknown, certain factors such as being over the age of 25 and having South Asian, East Asian, or Pacific Islander ancestry, may increase the risk. Other factors that may elevate the chances of developing gestational diabetes include:
- High blood pressure
- Heart disease
- Physical inactivity
- Family or personal history of GD
- Obesity
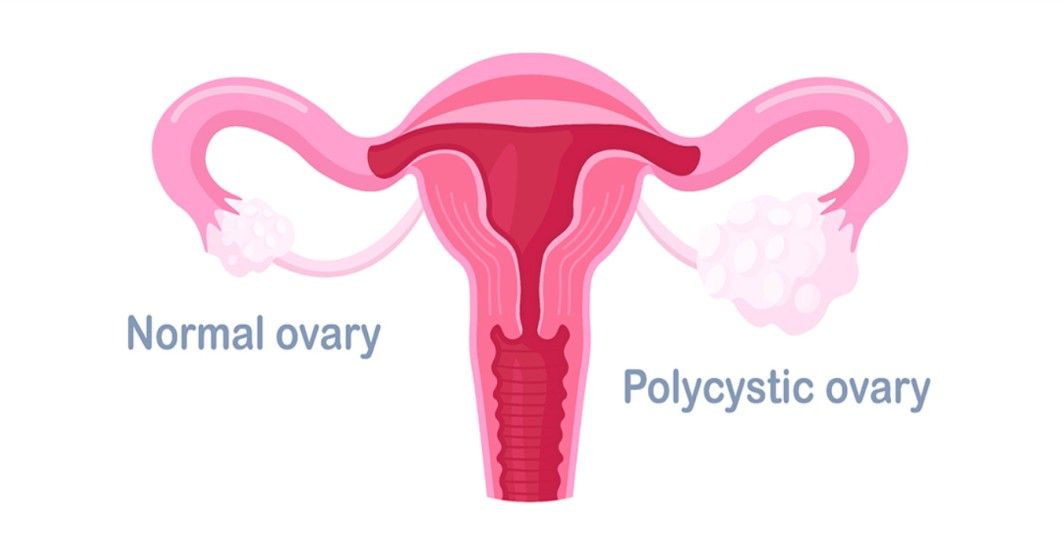
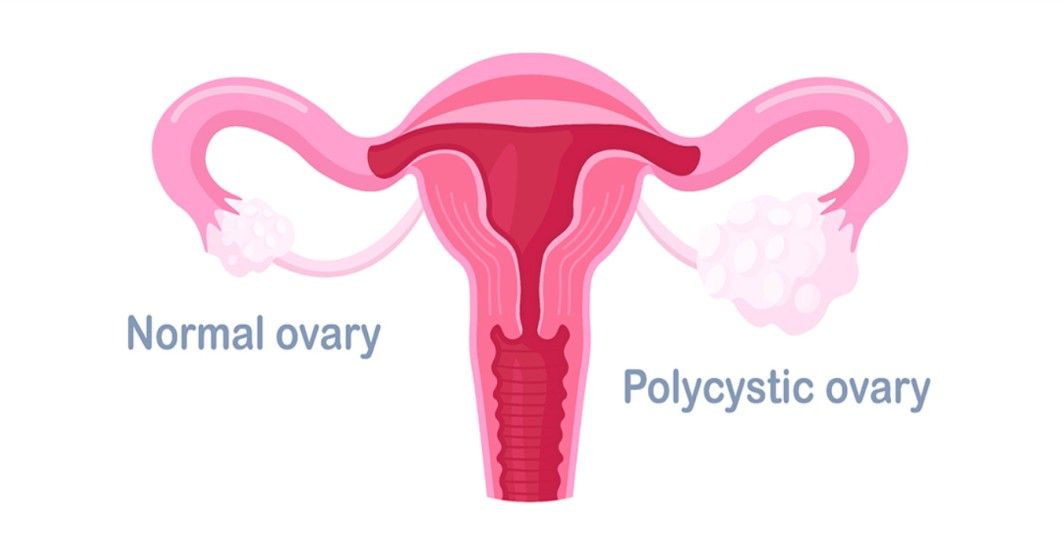
- Polycystic ovary syndrome (PCOS)
- Having an immediate family member who has diabetes
- Previous birth of a baby weighing over 4 kilograms
- Prediabetes
- Having multiple pregnancies
Gestational Diabetes Diagnosis
If you have an average risk of developing gestational diabetes, your doctor will conduct a test for the condition between weeks 24 and 28 of your pregnancy. To diagnose gestational diabetes, your healthcare provider will perform certain blood sugar tests, such as:
1. Glucose Challenge Test
During this test, you will be asked to drink a sweet liquid, and after approximately one hour, your blood sugar level will be checked with a blood test. A blood sugar level of 190 mg/dL indicates the presence of gestational diabetes. A blood sugar level below 140 mg/dL is generally considered normal for a glucose challenge test. If your blood sugar level is higher than normal, your healthcare provider will proceed with a glucose tolerance test.
2. Glucose Tolerance Test
An oral glucose tolerance test is conducted if your results from the glucose challenge test are abnormal. Before this test, you will need to fast for eight hours. Your healthcare provider will take blood samples 4 times; fasting state and at one, two, and three hours after you consume a sweet liquid. If at least two of the four blood sugar readings are higher than expected, the person is diagnosed with gestational diabetes.
Gestational Diabetes Treatment
Once you have been diagnosed with gestational diabetes, it cannot be cured or eliminated until the baby has been born. However, you can take steps to manage the condition and prevent serious complications.
If you have gestational diabetes, you may require more frequent checkups during the pregnancy. Your doctor will regularly monitor your blood sugar levels. You might also need to use a glucose meter at home to monitor your blood sugar.
In some cases, synthetic insulin may be necessary to manage gestational diabetes. However, most individuals can control their blood sugar levels through dietary changes and exercise. Here are some simple tips to help manage gestational diabetes:
- Focus on consuming vegetables, fruits, lean proteins, and whole grains. These foods are rich in nutrients and fiber while being low in calories and fat.
- Avoid junk food, sugary drinks, and processed foods as they can cause spikes in blood sugar levels.
- Strive for a balanced diet that includes a mix of proteins, fiber, carbohydrates, and healthy fats. This balance helps regulate blood sugar levels and provides essential nutrients for both you and your baby.
- Instead of having large meals, opt for smaller, frequent meals throughout the day. This approach helps maintain steady blood sugar levels.
- Establish a consistent meal schedule by eating at the same times each day. This routine can help regulate blood sugar and promote better overall control.
- Regular exercise is beneficial for lowering blood sugar levels. Consult with your healthcare provider to create a safe and suitable exercise plan for your specific needs.
- If prescribed, take all medications and insulin as directed and on time.
- Remember to work closely with your healthcare provider and seek their guidance to develop a personalized plan that aligns with your specific condition and needs.
Gestational Diabetes: Complications and Effect on the Baby
If left untreated and not managed properly, gestational diabetes can result in various complications for both the mother and the baby. Some potential risks associated with gestational diabetes include:
1. Caesarean Birth (C-section)
Women with gestational diabetes have a higher likelihood of delivering via C-section, especially if the baby grows too large.
2. Preeclampsia
Gestational diabetes increases the risk of developing high blood pressure and preeclampsia. Preeclampsia is a serious pregnancy complication characterized by high blood pressure and other symptoms that can pose risks to both the mother and the baby.
3. Type 2 Diabetes
If you've had gestational diabetes before, you have a higher chance of developing it again in future pregnancies. Additionally, there is an increased risk of developing type 2 diabetes later in life.
If you suffer from gestational diabetes, your baby is at an increased risk of the following complications:
1. Increased Birth Weight
Elevated blood sugar levels can cause the baby to grow larger than average. Babies weighing 4 kgs or more are at a higher risk of birth injuries, canal blockage, or requiring a C-section birth.
2. Premature Birth
High blood sugar levels may raise the likelihood of early labor and delivery before the due date. In some cases, early delivery might be recommended if the baby's size poses a risk.
3. Breathing Problems at the Time of Birth
Babies born prematurely may experience respiratory distress syndrome, which is a condition that makes breathing challenging.
4. Hypoglycemia
Newborns may have hypoglycemia, or low blood sugar levels, shortly after birth. Severe cases of hypoglycemia can lead to seizures. Feeding the baby promptly or providing an intravenous glucose solution can help restore normal blood sugar levels.
5. Obesity or Type 2 Diabetes
Babies born to mothers with gestational diabetes have a higher likelihood of developing type 2 diabetes and obesity in the future.
6. Stillbirth
If gestational diabetes remains untreated, it can increase the risk of stillbirth, which refers to the death of the baby either before or soon after birth.
Is Gestational Diabetes Preventable?
While it's not possible to completely prevent gestational diabetes, there are steps you can take to reduce your risk of developing the condition. These healthy choices may also lower the chances of developing gestational diabetes in future pregnancies or type 2 diabetes later in life:
1. Eat a Healthy Diet
Focus on consuming foods that are rich in fiber and low in calories and fat. Increase the intake of vegetables, fruits, and whole grains. Aim for variety to maintain a balance of nutrition and taste. Be mindful of portion sizes and watch your overall calorie intake.
2. Stay Physically Active
Engaging in regular exercise before and during pregnancy can help lower the risk of gestational diabetes. Strive for at least 30 minutes of moderate exercise on most days of the week. Ride a bike, take brisk walks, swim laps, or find other activities you enjoy. Even small bursts of activity, like taking short walks or parking farther away, can make a difference.
3. Start Your Pregnancy at a Healthy Weight
If you're planning to become pregnant, it can be beneficial to achieve a healthy weight beforehand. Losing any excess weight and adopting healthier eating habits can contribute to a healthier pregnancy.
4. Control Weight Gain
It's normal and necessary to gain weight during pregnancy, but excessive weight gain can increase the risk of developing gestational diabetes. Consult with your healthcare provider to determine the appropriate amount of weight gain for your specific situation.
Summary
It is advisable to seek healthcare early, especially when you are considering getting pregnant. By doing so, your healthcare provider can assess your risk of developing gestational diabetes and ensure your overall well-being. During your prenatal care, your provider will routinely screen you for gestational diabetes. If you are diagnosed with gestational diabetes, you may require more frequent checkups, particularly in the final three months of pregnancy. Your healthcare provider will closely monitor your blood sugar levels and the well-being of your baby during this time.
For more information, Consult Apollo’s Expert Diabetologists
FAQs
Q. What happens if I am diagnosed with gestational diabetes?
If diagnosed with gestational diabetes, your healthcare provider may refer you to a nutritionist for dietary adjustments and blood sugar monitoring. Your obstetrician will develop a management plan, including more prenatal visits to monitor fetal growth, weight gain, and blood sugar control. So, talk to your doctor about checking your blood sugar and what your levels should be after meals.
Q. Is diet responsible for gestational diabetes?
While diet can contribute to the development of gestational diabetes, it is important to note that it does not directly cause diabetes. Gestational diabetes occurs when hormones from the placenta hinder the body's ability to use or produce insulin.
Q. Can I still have a healthy pregnancy if I am diagnosed with gestational diabetes?
Yes, having gestational diabetes doesn't mean you cannot have a healthy pregnancy and a healthy baby. This condition is highly treatable and manageable. It's important to collaborate with your doctor to fully comprehend your treatment plan and learn how to maintain healthy blood sugar levels.
Q. Does gestational diabetes always go away after childbirth?
After giving birth, your blood sugar levels should return to normal as your hormone levels stabilize. However, it's important to note that approximately 50% of individuals with gestational diabetes will get Type 2 diabetes in the future. To lower your risk, maintaining a healthy diet and engaging in regular exercise are recommended. Your doctor may suggest blood glucose tests every 6 to 12 weeks following pregnancy to monitor for the development of diabetes.
Q. Is exercising safe during pregnancy?
Yes, exercising during pregnancy is not only safe but also advisable unless your doctor has suggested otherwise. You can consult your doctor to help create a safe and effective exercise plan for you based on your age, weight, overall health, and fitness levels before pregnancy.
Medically reviewed by Dr Sonia Bhatt.
Diabetes Management
Consult Top Dieticians
View AllLeave Comment
Recommended for you

Diabetes Management
Can Diabetes Affect Your Recovery?
Diabetes impacts recovery, leading to delayed healing, infection risks, and surgical complications due to impaired blood flow and immune function. Neuropathy complicates pain management, while comorbidities extend recovery times. Effective management, including blood sugar control and a healthy lifestyle, improves outcomes. High blood sugar limits healing by reducing nutrient flow and immunity, promoting inflammation.
Diabetes Management
The Link between Prediabetes and Polycystic Ovary Syndrome (PCOS)
With nearly 30% to 40% of women with PCOS also having prediabetes, awareness and effective management are key as thiisalso raises the risk of type 2 diabetes and heart disease. The good news is that lifestyle changes, medication, and regular monitoring can significantly reduce the risk and improve overall health.

Diabetes Management
The Dangers of Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes characterized by high blood sugar, dehydration, and acidosis. It can lead to organ failure, coma, and even death if not treated promptly. Symptoms include excessive thirst, frequent urination, and fruity breath odour. Immediate medical attention is crucial to treat DKA and restore electrolyte balance.
Subscribe
Sign up for our free Health Library Daily Newsletter
Get doctor-approved health tips, news, and more.
Visual Stories

8 Fruits That are Incredibly Healthy for Diabetes
Tap to continue exploring
Recommended for you

Diabetes Management
Can Diabetes Affect Your Recovery?
Diabetes impacts recovery, leading to delayed healing, infection risks, and surgical complications due to impaired blood flow and immune function. Neuropathy complicates pain management, while comorbidities extend recovery times. Effective management, including blood sugar control and a healthy lifestyle, improves outcomes. High blood sugar limits healing by reducing nutrient flow and immunity, promoting inflammation.
Diabetes Management
The Link between Prediabetes and Polycystic Ovary Syndrome (PCOS)
With nearly 30% to 40% of women with PCOS also having prediabetes, awareness and effective management are key as thiisalso raises the risk of type 2 diabetes and heart disease. The good news is that lifestyle changes, medication, and regular monitoring can significantly reduce the risk and improve overall health.

Diabetes Management
The Dangers of Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA) is a life-threatening complication of diabetes characterized by high blood sugar, dehydration, and acidosis. It can lead to organ failure, coma, and even death if not treated promptly. Symptoms include excessive thirst, frequent urination, and fruity breath odour. Immediate medical attention is crucial to treat DKA and restore electrolyte balance.


